Clinical Assessment Workgroup
Clinical assessment at UWSOM is changing!
New workplace-based assessments are coming to required Patient Care Phase core clerkships in Spring 2025
Pass/Fail grading is coming to required Patient Care Phase core clerkships in Spring 2026
Why change?
As part of a national movement toward competency-based medical education (CBME), UWSOM is changing its assessment and grading practices in the clinical phases to better align with patient needs and physician competencies. The need for change is driven by several key factors:
- Patient-Centered Focus: The curriculum and assessments will be designed to align with patient needs, emphasizing the competencies that characterize effective physicians.
- Equity in Grading: Current grading practices have highlighted inequities related to race, ethnicity, and gender, necessitating a more equitable approach.
- Transparency: The existing grading system lacks clarity, which can hinder student learning. The new CBME assessment model, featuring pass/fail grading, aims to foster trust and enhance communication regarding student achievements.
- Ongoing Development: CBME encourages continuous growth through self-directed learning and reflective practice, enabling students to develop their skills progressively and prepare for the transition to graduate medical education (GME).
- Focus on Competence: The updated assessment framework will prioritize meaningful evaluations of student competence, shifting the emphasis from traditional grades to practical, real-world patient care.
- Reduction of Bias: By minimizing peer comparisons and concentrating on formative feedback, the School aims to establish a more equitable assessment process.
Overall, these changes reflect a commitment to fostering an educational environment that supports professional growth, reduces bias, and ensures that all students are prepared to meet the needs of their future patients.
How did we get here?
On March 7, 2022, the UWSOM Curriculum Committee, acting upon the recommendations of the Program Evaluation and Assessment Committee (PEAC) and feedback from the Patient Care Committee, charged a workgroup to explore making broad changes to clerkship grading, centering equity and transparency.
The charge included the need to:
- Create an equitable assessment strategy
- Center transparency
- Implement competency-based assessments
- Assess a comprehensive and holistic skill set
- Make the MSPE reflect assessment
- Encourage a growth mindset/lifelong learning
It was additionally determined that the initial implementation of any changes to the clinical assessment system would be limited to required third- and fourth-year clerkships.
Members of the Clinical Assessment Workgroup were recruited from a wide range of stakeholders. A list of current workgroup members is below:
| NAME | ROLE |
|---|---|
| Phaedra Allen | Business Analyst, ALT |
| Erikka Allhusen | Faculty, Pediatrics |
| Ayana Amaechi | MS3, Idaho |
| Amy Baernstein | Chair, Student Progress Committee; Faculty, Medicine |
| Frank Batcha | Co-Director, WRITE Program; Assistant Clinical Dean, Idaho |
| Justin Bullock | UW Fellow, Nephrology |
| Markus Boos | Program Director, Dermatology |
| Paul Borghesani | Clerkship Director, Psychiatry |
| Bekah Burns | Clerkship Director, Pediatrics |
| Sarah Byquist | MS3, Spokane |
| Andrea Cabarello | College Head, Alaska |
| Julie Calcavecchia | Director, FCM & The Colleges |
| Kris Calhoun | Clerkship Director, Surgery |
| Michael Campion | Director, ALT |
| Andy Castrodale | Site Lead, Family Medicine |
| Esther Chung | Director, Advanced Patient Care Clerkships |
| Adam Crandall | MS3, Idaho |
| Erica Crittendon | MS3, Seattle |
| Matt Cunningham | Director, Educational Evaluation |
| Jake Dahl | Clerkship Director, Otolaryngology Head & Neck Surgery |
| Sophia Deklotz | MS4, Idaho |
| Neha Deshpande | Clerkship Director, Internal Medicine |
| Amy Dettori | Associate Clerkship Director, Pediatrics |
| Aleksei Dingel | MS4, Idaho |
| Kellie Engle | Director, Curriculum |
| Jay Erickson | Assistant Clinical Dean, Montana |
| Sara Fear | Clerkship Administrator, Pediatrics |
| Gina Franco | Assistant Director, Curriculum |
| Douglas Franzen | Program Director, Emergency Medicine |
| Fiona Gallahue | Program Director, Emergency Medicine |
| Jacob Gross | Clerkship Director - APCs, Anesthesiology |
| Emina Gulbis | MS3, Idaho |
| Josiah Hanson | Clerkship Director, Dermatology |
| RaQuel Harwick | Clerkship Administrator, Obstetrics & Gynecology |
| Ivan Henson | Clerkship Administrator - Sub-Is, Family Medicine |
| Molly Jackson | Assistant Dean, The Colleges |
| Joshua Jauregui | Assistant Dean, Clinical Curriculum |
| Geoff Jones | Assistant Clinical Dean, Spokane |
| Karla Kelly | Program Operations Specialist, Learning Environment |
| Mallory Kester | E&F Clerkship Administrator, Internal Medicine |
| Toby Keys | Clerkship Director, Family Medicine |
| Sarubh Khandelwal | Faculty, Surgery |
| Meghan Kiefer | Director, Educational Experience |
| Jordan Kinder | Manager, Curriculum Management System |
| Elana King-Nakaoka | MS3, Idaho |
| Chris Knight | UWMC Faculty, Internal Medicine |
| Amanda Kost | Co-Director, WRITE Program; Faculty, Family Medicine |
| Eric Kraus | Clerkship Director, Neurology |
| Christopher Kweon | Program Director, Orthopedic Surgery |
| Andrea Larson | MS3, Spokane |
| Aidan Loeser | MS3, Seattle |
| Justin Magee | Research Scientist, BIME |
| Erik Malmberg | Assistant Dean, Equity & Medical Student Engagement |
| Carmelita Mason-Richardson | Clerkship Administrator, Medicine |
| Karen McDonough | Director, FCM |
| Heather McPhillips | Associate Dean, Curriculum |
| Vicky Mediratta | Clerkship Director, Obstetrics & Gynecology |
| Susan Merel | Clerkship Director - E&F Clerkships, Medicine |
| Som Mookherjee | Director, CLIME; Faculty, Cascade College |
| Carl Morris | Liaison, Kaiser Permanente |
| Tom Moynihan | Manager, Departmental Computing, DOM IT |
| Sheva Mozafari | MS3, Idaho |
| Linh Ngo | Career Advisor |
| Lan Nguyen | Clerkship Administrator, Dermatology |
| Kim O'Connor | Clinical Learning Specialist; Faculty, Cascade College |
| Doug Paauw | Clinical Learning Specialist; Faculty, Medicine |
| Pam Pentin | Clerkship Director - APCs & Sub-Is, Family Medicine |
| Darryl Potyk | Associate Dean, Eastern Washington |
| Melissa Riesland | Specialist, MSPE |
| Maya Sardesai | Assistant Dean, Student Development |
| Caitlin Schrepel | Assistant Program Director, Emergency Medicine |
| Robin Scott | Educator, WRITE |
| Alicia Scribner | Site Director, Madigan |
| Kristen Seiler | Clerkship Administrator, Surgery |
| Katie Sexton | MS3, Seattle |
| Samartha Shrestha | MS3, Spokane |
| Isha Shrestha | MS3, Seattle |
| Sam Simpson | MS4, Idaho |
| Mathew Sorenson | Program Director, Urology |
| Ken Steinberg | Program Director, Medicine |
| Rachel Straughn | MS3, Seattle |
| Sarah Thomson | Career Advisor |
| Sarah Villareal | Assistant Clerkship Director, Obstetrics & Gynecology |
| Christen White | Assistant Director, ALT |
| Sarah Wood | Director, Student Affairs |
| Jenny Wright | Clerkship Director, Medicine |
| Melissa Zent | Manager, MSPE |
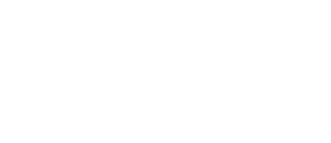
Project Timeline
Project Phases & Reports
The project encompasses the 4 phases detailed below and is currently slated for initial implementation in Spring 2025. Below you will find important project information and details as we aim for, progress toward, and achieve project milestones. Make sure to visit often as information will be updated regularly.
December 2022 – May 2023
Workgroup members from Phase I defined the guiding principles for the new assessment strategy and explored models of assessment, including both programmatic assessment programs (e.g., CBME) and methods of assessment (e.g., workplace-based assessments). They ultimately recommended that all required clerkships be converted to a pass/fail grading system, with the additional recommendation that the clinical assessment system be reworked with a competency-based medical education (CBME) focus, utilizing entrustable professional activities (EPAs) as a workplace-based assessment. Those recommendations were unanimously approved in Autumn 2023 by UWSOM Curriculum governance committees and the Faculty Council on Academic Affairs (FCAA).
Phase Milestones
- Recruit a Clinical Assessment Workgroup
- Review reasons for change
- Define the overarching values, goals, and measurable outcomes for a new assessment system
- Select a model for clinical assessment
Meetings
- December 15, 2022 – Phase 1 Kickoff Meeting
- January 11, 2023 – Workgroup Meeting 2
- February 13, 2023 – Expert talk from Dan Schumacher
- March 8, 2023 – Workgroup Meeting 3 with expert talk from Karen Hauer
- March 4, 2023 – CLIME Grand Rounds: Justin Bullock
- March 13, 2023 – Expert talk from Bob Englander
- March 28, 2023 – CLIME Grand Rounds: Jason Frank
- May 3, 2023 – Workgroup Meeting 4
- Phase 1 Summary Report
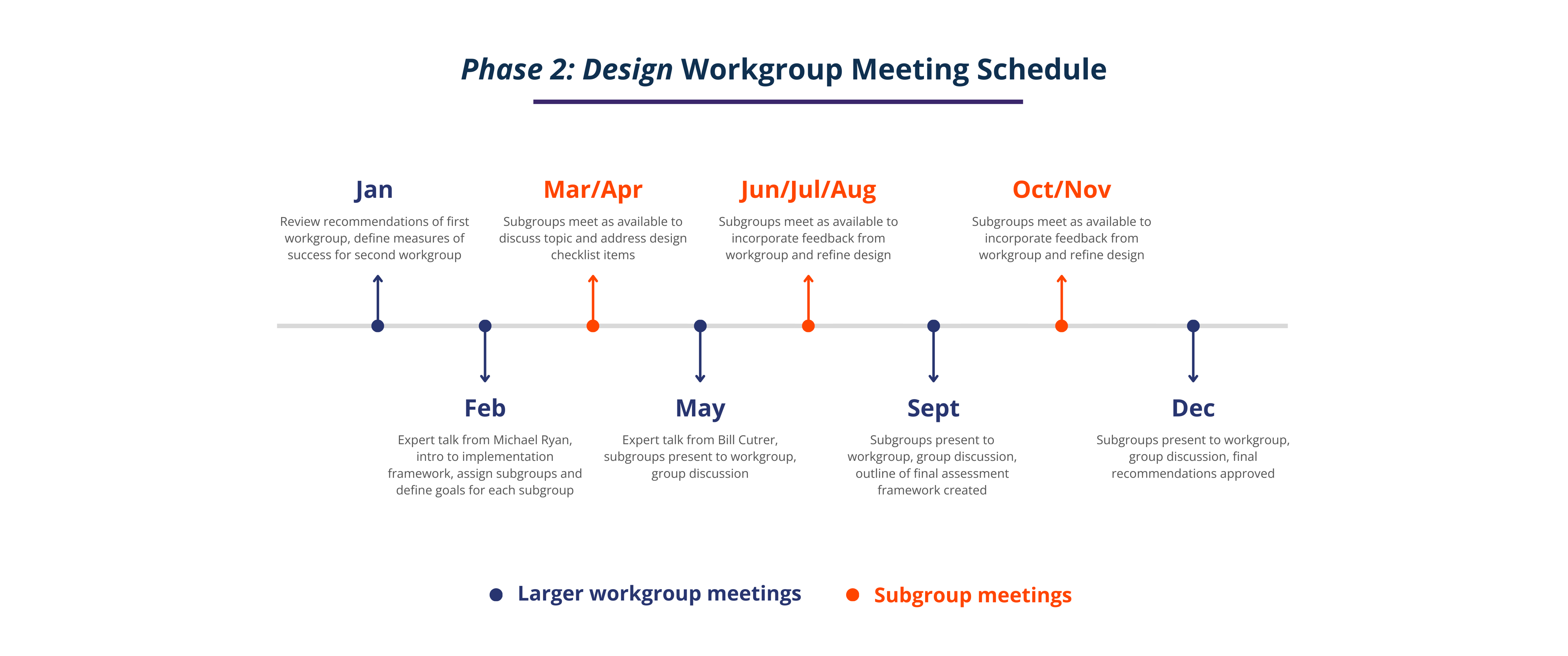
September 2023 – December 2024
Phase 2 of the Clinical Assessment Workgroup is scheduled to be completed by December 2024 and includes members of the first workgroup as well as additional stakeholders who will be impacted by changes to clinical assessment in required clerkships. This phase of the workgroup will define the components of the clinical assessment system for required clerkships, including:
- A comprehensive set of milestones based on CLOOM’s revised program objectives
- A set of longitudinally-assessed EPAs, including their use, timing, and any required revisions to clerkship curriculum
- The structure and role of clinical competency committees
- Requirements for and intended use of the technology support systems necessary for monitoring student progress across the curriculum
- A model for coaching to competencies
- A guide for determining clerkship grades, including suggested criteria and a standardized decision-making process
- Requirements for faculty development around CBME, EPAs, and the new clinical assessment system
- A strategy for addressing anticipated downstream effects on APCs and electives
It will also develop an implementation strategy for instituting pass/fail grading that aligns with planned changes to the clinical assessment system.
Five subgroups have been selected to facilitate broad participation and collaboration across key stakeholder groups. Each subgroup, charged with one or more of the strategic priorities identified above, have received terms of reference that define their purpose, mandate, timeline, and deliverables. The charge of these subgroups is centered on reviewing the medical education research literature and/or completing an environmental scan and then developing recommendations for review by the larger workgroup. Recommendations will then be presented to the Curriculum Committee and FCAA for approval.
Click here for more information about each subgroup’s charge.
Phase Milestones
- Launch subgroups to determine components of new assessment system
- Identify core roles and assign responsibilities
- Inventory available resources and request funding for additional required infrastructure
- Create new and/or alter existing supporting infrastructure
- Create a staged implementation plan
- Create a strategic plan for downstream effects of new assessment system
- Adapt required clerkship curriculum to fit with new assessment system
- Create robust resource guides and training materials
- Familiarize faculty, staff, and students with upcoming changes
- Submit all recommended changes to Curriculum governance, FCAA, and/or UW Provost by December 2024
Meetings
- September 2023 – January 2024 – Topic Engagement Meetings
- January 31, 2024 – Phase 2 Kickoff Meeting
- February 14, 2024 – Workgroup Meeting 2 with Expert Talk from Michael Ryan
- May 29, 2024 – Workgroup Meeting 3 with Expert Talk from Bill Cutrer, Subgroup Presentations
- September 19, 2024 – Workgroup Meeting 4
- December 6, 2024 – Workgroup Meeting 5
Spring 2025
Phase Milestones
- Implement approved changes to curriculum
- Implement new assessment methods
- Implement technology support systems
- Build faculty education and program evaluation strategies
The phased rollout plan for the new system of clinical assessment consists of 2 stages:
Trial Year 2025-2026
- EPAs are assessed as workplace-based assessments in all core required clerkships on a formative basis only. (There will be some latitude in the number of EPAs assessed within each clerkship, but the form will be consistent across clerkships.)
- Data gathered from EPA assessments is used to train newly established coaches and CCCs beginning November 2025. CCCs map to milestones using EPA assessments for formative purposes only.
- Additional technology support systems, training and development programs, and clinical remediation requirements are developed.
- Clerkship assessment requirements are revised to include EPAs and are mapped to milestones.
- Changes are presented for Curriculum Committee review and approval.
Watch the video below to learn more about WBAs, including guidance on how to complete a WBA. Practice submitting a sample WBA form as you watch to familiarize yourself with the process.
Go Live Year 2026-2027
- Grading in all core required clerkships goes Pass/Fail.
- Longitudinal clerkship assessment data, including EPAs, is reviewed by CCCs to determine promotion/remediation recommendations.
Meetings
- June 25, 2025 – Workgroup Meeting 1
- September 26, 2025 – Workgroup Meeting 2
- December 2, 2025 – Workgroup Meeting 3
2027 –
Phase Milestones
- Make adjustments to initial implementation plans and processes as needed
- Track and monitor data to ensure desired outcomes are achieved
- Solicit feedback from stakeholders and other end users
- Identify areas for improvement
FAQs
CBME is an approach to preparing physicians for practice that is fundamentally oriented to graduate outcome abilities and organized around competencies derived from an analysis of societal and patient needs. This outcomes-based approach to the design, implementation, assessment, and evaluation of a medical education program is structured around a framework of competencies (e.g., AAMC Physician Competency Reference Set). Curriculum is organized around the outcomes expected of a medical student and a student’s advancement is dependent on having achieved those expected outcomes.
CBME Core Components:
- An outcomes competency framework
- Progressive sequencing of competencies
- Learning experiences tailored to competencies
- Teaching tailored to competencies
- Programmatic assessment
An entrustable professional activity (EPA) is a key task of a discipline (i.e. specialty or subspecialty) that an individual can be trusted to perform in a given health care context once sufficient competence has been demonstrated. EPAs are a common approach to CBME around the world. EPAs are linked to a specific stage of the competence continuum and integrate multiple milestones from various roles.
Some people think of an EPA as a basket or a bundle that holds numerous milestones. As students progress through the stages of the continuum, the EPAs become progressively more complex, reflecting students’ achievement of more sophisticated milestones.
The WWAMI Rural Integrated Training Experience (WRITE) program began using EPAs in Spring 2023. Preceptors use a student-generated survey to indicate entrustment level, context of encounter, and give formative feedback.
A milestone is an observable marker of an individual’s ability at a stage of expertise. Milestones illustrate the expected progression of competence from novice to mastery associated with each enabling competency.
Milestones:
- Illustrate the developmental nature, features, and progression of the competencies
- Assist learners in monitoring their own developmental progress
- Allow individuals to monitor their own progress
- Support the identification of learners whose progress is not following the typical development sequence to assist in early intervention
- Guide curriculum development
Questions? Contact Mary Sargent, sargem@uw.edu.